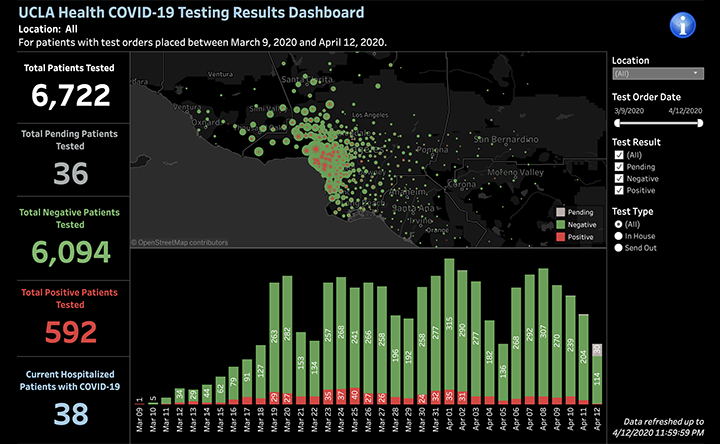
54000 test for 9000 cases means you can test 6 negatives for each positive. If you manage to use that wisely, it can work out.
Covid-19 is contagious even if you are not showing symptoms, that's why it's so dangerous. Your argument of "testing is only needed on a selected number of patients" is what led the pandemic to where it is right now.
From your source:
External Quote:
widespread testing helped Taiwan, South Korea and Germany blunt the epidemic's rise.
I'm from Germany, I know how we have been testing because the guidelines are public. We are also screening respiratory illnesses:
External Quote:
In der 13. KW sind in zwei von insgesamt 121 untersuchten Sentinelproben (1,7 %) SARS-CoV-2 identifiziert worden.
https://influenza.rki.de/Wochenberichte/2019_2020/2020-13.pdf
This says that in the week 21-27 March, 121 samples of persons with symptoms were tested for all kinds of viruses, and only 1.7% had coronavirus. You need 60 times more tests than cases if you want to test everyone with symptoms.According to the article you linked, we are doing the most testing per capita in the world, but even we don't have that.
Instead, besides treatment tests on people who present with pneumonia, we tested people who have symptoms and a link to an infection source, or people who have symptoms and have high risk (e.g. doctors). This supports contact tracing and containment. Contact tracing and containment is how South Korea managed its epidemic. Note also that Taiwan is an island, and South Korea is a peninsula witha fairly tight border to the North; while Germany has open borders and many Germans went skiing in the Alps in Italy or in Austria next to the Italian border and brought Covid home. In my town, 5 such vacationers developed symptoms on the way home, their group was tested, they were identified and quarantined.
You can't use the tests to test everyone who is fearful and afraid, it just is not possible. You need to use them wisely, or you don't have enough where they can really make a difference: where you need to identify and contain a local spread one infection at a time.
The "per capita" test rate is indicative of potential, but what you want is a good "per case" test rate that allows you to keep track of the people whom your identified cases might have infected, and who these might have infected, etc. I don't know if there are data on this, but my impression is that this should be possible if your tests come back 5%-10% positive. So your 15% is cause for concern, but not the end of the world.
The problem with ramping up testing is that you need expensive lab equipment and medical technicians to run it. A lab machine can do 96 tests in 4-6 hours if you have the chemicals, but at a certain point, you need to buy more machines and train more people to operate them. You can't just demand more tests and expect them to happen. Germany has many independent labs; the labs have been learning this process since January and have been increasing their capacities, but we're starting to run out of chemicals.
What you need to achieve in Brazil is to keep the infection rate down so that quarantine measures (based on tests) have a chance to contain the spread again and again. Contact tracing is the only way to let people know they might be infectious before they have symptoms; that is the path to containment, and containment is the way out of this crisis.
(The other way is to push the transmission rate from R=5.2 to R=0.58 and wait a few weeks, as Wuhan has done with their strict quarantine measures, and today China uses an app to do contact tracing and quarantine. It appears to be working.)
Keep a diary on whom you were in contact <6 feet unprotected, and for how long. If you develop Covid-19, go back two days from the onset of symptoms; some of the people you had contact with for more than 15 minutes will have been infected by you.
If social distancing reduces the contacts everyone has, you do not need as many tests to do thorough contact tracing, because there aren't as many contacts for each case. These measure reduce the number of test per case. Do it well and you can beat the virus!