Image Source: https://www.bostonglobe.com/metro/2...regan/4fttzx4spJ8SRA8GQLAWuI/story.html?pic=9
This is Boston bombing victim Marc Fucarile. He spent 45 days at mass general, 55 at Spaulding for rehab. Had right leg amputated, severe injuries to left leg including burns and fractured foot. These are from The Boston Globe, here is a link confirming that the top picture was taken when was transferred to Spaulding, scroll to number 5 the bottom pic is from Mass General http://www.bostonglobe.com/metro/20...regan/4fttzx4spJ8SRA8GQLAWuI/story.html?pic=9 Notice his stump in the bottom pic, despite some discoloration it looks like it's healing nicely and probably pretty far along in his stay. Which is great because in order to get transferred to rehab you need to be well healed.
However, notice the stump in the top picture where he is supposedly getting physical therapy at Spaulding. His stump is no longer healthy, in fact the color can only mean one thing, gangrene. How did his well healed stump turn to gangrene? And if it is truly gangrene, why would they release him from the hospital, it's kind of an emergent situation he could get septic and die- you take him to surgery, you don't do physical therapy on an amputee with a gangrenous stump.
Mod: the black is the foam dressing used in negative pressure wound therapy:
https://en.wikipedia.org/wiki/Negative-pressure_wound_therapy
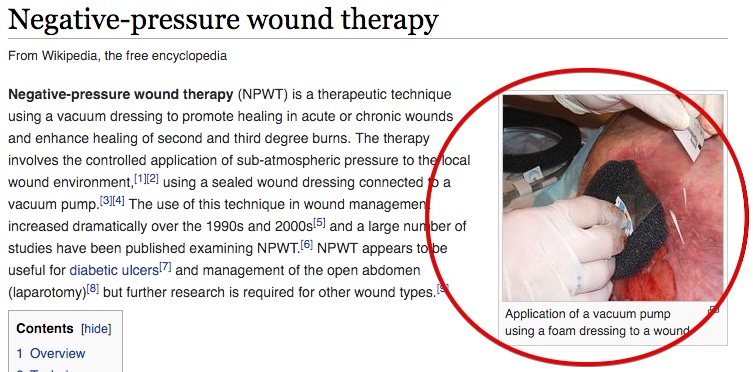
https://en.wikipedia.org/wiki/Negative-pressure_wound_therapy
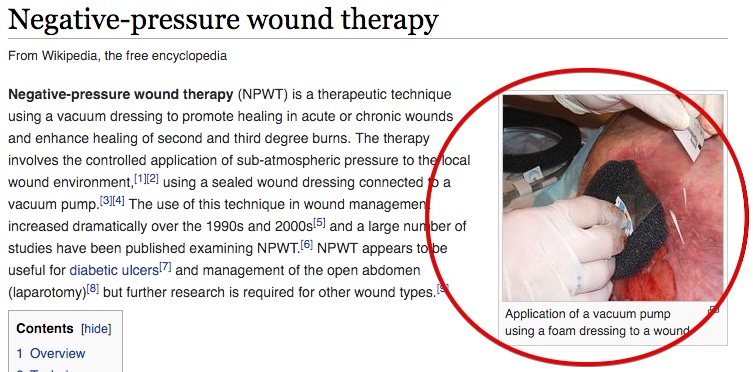
Also notice it's covered in plastic with a tube coming from it, pretty sure that's "vacuum assisted wound closure" therapy VAC, where it produces negative pressure or suction to help certain wounds heal. The only problem is VAC is contraindicated in gangrene, you have to debride all the black dead tissue away before can use VAC.
Mod: See above, VAC is Negative-pressure wound therapy
Also notice the large tube sticking out of the bandages on the left, again he would not have released him and be doing physical therapy on him if he had kind of seeping infected wound requiring such a drain! I can't even imagine what it's supposed to be draining, he had severe burns, but even if they were fresh and seeping you dress them you don't stick a giant tube to drain burns. The only thing I can think of that would require such a tube would be if he had an infected surgical wound of some type, which makes no sense if he's in rehab.
Mod: It's the same tube going into the NPWT
One more thing that does not make sense, in the second picture he has a nasogastric tube in. NG tubes have limited applications- to feed patients food or drugs because they can't swallow for some reason, or to decompress the GI tract in a patient with bowel obstruction and things are back up the wrong way. In the latter case the patient would likely be in severe pain and on his way to surgery, not sitting comfortably in bed. So why does he have a nasogastric tube? Am I missing something? I can provide links for any of the above, first post not sure what I need to substantiate with links, in this post the pictures pretty much speak for themselves.
Mod: There are multiple reasons, see below.
Last edited by a moderator:


